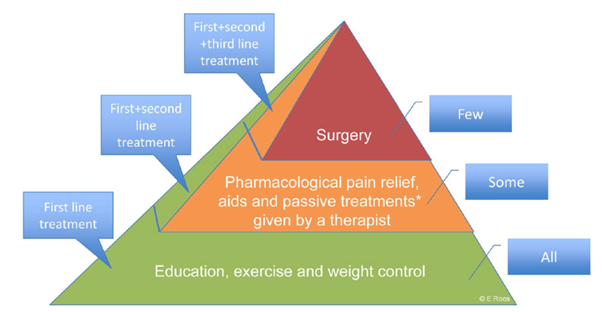
Despite education, exercise and weight loss (if needed) being first line/core treatment options. Some patients may require a little extra assistance to control symptoms.
 A brace can help ease loads on the joint. Knee braces surround the joint and make it more stable.
A brace can help ease loads on the joint. Knee braces surround the joint and make it more stable.
Some people may need to change the load pattern on the foot or knee with insoles from an orthopedic shoemaker or physiotherapist. If you are limping, a walking aid, such as a cane or Nordic walking poles, can help ease the pain and prevent straining other joints.
 Paracetamol (for example Panadol, Tylenol) is usually the first choice for pain relief for osteoarthritis. It gives the fewest side effects and can be used as needed. Too much can damage the liver, therefore you should not go over the prescribed dose.
Paracetamol (for example Panadol, Tylenol) is usually the first choice for pain relief for osteoarthritis. It gives the fewest side effects and can be used as needed. Too much can damage the liver, therefore you should not go over the prescribed dose.
Ibuprofen (for example Motrin, Advil and Naproxen) can be used when Paracetamol is not working well enough. These can also be used if the joints are hot and swollen. Both drugs reduce pain, swelling and stiffness. There is a low chance that these drugs can cause a side effect in the stomach. Therefore, they are not suggested for those with ulcers. Theses drugs have also been seen to raise the risk of some heart diseases.
 Platelet-rich plasma injection (PRP injection) aims to stimulate cartilage repair and offer relief to other osteoarthritic symptoms, potentially delaying the need for joint replacement surgery. PRP injections have shown to influence the entire joint environment, leading to a short-term clinical improvement.
Platelet-rich plasma injection (PRP injection) aims to stimulate cartilage repair and offer relief to other osteoarthritic symptoms, potentially delaying the need for joint replacement surgery. PRP injections have shown to influence the entire joint environment, leading to a short-term clinical improvement.
Corticosteroid injection (cortisone) may also be used if the joint is hot and swollen. This can decrease pain in 1-4 weeks. Research has not found any long-term effects from corticosteroid injections. An injection of corticosteroid medication into the joint during a ‘flare’ can provide short-term pain relief and help you return to an exercise program or normal activity.
Hyaluronic acid (HA) can be useful for those with mild to moderate osteoarthritis in reducing pain, swelling and stiffness. In a joint affected by osteoarthritis, there is less naturally occurring hyaluronic acid and it can be less viscous than in a normal healthy joint. Injecting hyaluronic acid directly into a joint raises its levels, which can ease pain and improve joint function.
Surgery is at the top of the treatment pyramid.  Most people can control their osteoarthritis with other forms of treatment. If this is not possible, surgery may be needed. Only 10-15% of people with osteoarthritis will need surgery.
Most people can control their osteoarthritis with other forms of treatment. If this is not possible, surgery may be needed. Only 10-15% of people with osteoarthritis will need surgery.
Arthroplasty/Joint replacement
Metal or plastic artificial joint surfaces replace the damaged joint. This surgery is most common in the hip, knee and some fingers. Clinical guidelines in Australia recommend considering joint replacement surgery for severe osteoarthritis if all conservative treatment options have failed (RACGP 2018). The advantage of this surgery is that pain lessens or stops completely. Often, range of motion in this joint is still slightly limited. All joint replacements require correction (revision surgery) over time. This is more difficult than the initial surgery because the surgeon must remove the old joint. There may be scar tissue, and the person’s bones may not be as strong as they were. Therefore, revision surgery has a higher risk of complications, and recovery usually takes longer.
Osteotomy
In severe deformities like knock knee or bow-leg, only one part of the knee has thin or no articular cartilage. The other parts of the knee are well. In this case, osteotomy can help. Osteotomy takes a wedge of bone from the lower leg bone, straightening the leg. This helps to change the load so that the part of the knee with osteoarthritis doesn’t take as much load. A metal plate and screws are used to support the bone so that it heals properly.
Arthroscopy (keyhole surgery)
For most people with osteoarthritis (OA), arthroscopy is not recommended as a treatment for pain. Recent research indicates that its benefits in reducing pain are no better than a placebo for people with OA (a placebo is a ‘fake’ treatment with no known medical effects, such as sterile water or a sugar pill). During an arthroscopy, your doctor looks at the inside of your joint by passing an instrument called an arthroscope into the joint. The doctor may then use small surgical instruments (probes, scissors, shavers) to perform tasks such as removing or repairing torn ligaments, tendons or cartilage, or other minor surgery.
Physiotherapist
 A physiotherapist is a skilled health professional in the understanding of body movement and function. A physiotherapist can help with:
A physiotherapist is a skilled health professional in the understanding of body movement and function. A physiotherapist can help with:
- Assessment. A physiotherapist can assess your joint difficulties, your function and your level of activity. This will help them find a treatment that fits you best.
- Exercise. A physiotherapist can help you find the right ways to exercise and adjust the exercises to your needs.
- Knowledge. You can get advice if you’re unsure of how to exercise or how it should feel when exercising.
- Pain relief. The physiotherapist has tools that may ease your joint pain so that you can proceed with your exercises.
- Walking Aids. If needed, the physiotherapist can help you get a walking aid if your joint is painful and needs relief.
- Inspiration and motivation. It can be hard to get started if you haven’t exercised for a while or if you are in pain. Starting with a physiotherapist for 6-8 weeks can help you shift into an active lifestyle.
This ABC article may help you to understand the differences among Physiotherapist, Chiropractor, Osteopath, and Myotherapist:
General practitioner (GP)
 GPs are usually the first point of contact with the health care system for people with osteoarthritis. A GP can help with:
GPs are usually the first point of contact with the health care system for people with osteoarthritis. A GP can help with:
- Initial diagnosis of osteoarthritis.
- Referring you to a specialist (rheumatologist), other health professionals and services.
- Prescribing medication.
Dietitian

A dietitian can give you tailored advice to assist with your nutritional health:
- Helping you to lose weight (if necessary), which can help to reduce your symptoms and slow osteoarthritis progression
- Reducing raised blood cholesterol and increasing intake of rich vitamin K sources may benefit OA.
- Achieving adequate levels of vitamins A, C and E
Orthopaedic Surgeon

If you have tried other treatments including exercise and weight management (if appropriate), if your knee osteoarthritis is advanced and, if symptoms can no longer be tolerated, surgery is an option.
The surgeon will assess whether joint replacement is likely to work for you, including how fit you are and any other medical conditions that might rule out surgery.

